Drugged seniors were prescribed by doctors: Minister
In a heated scrum at Queen’s Park on Tuesday, Health Minister Deb Matthews blamed doctors for prescribing powerful antipsychotic drugs to elderly in nursing homes.


Ontario Health Minister Deb Matthews acknowledged the drugging of seniors in provincially regulated nursing homes is a problem but suggested doctors are responsible.
“Let’s remember, it’s doctors who prescribe these drugs, not the government,” Matthews told reporters in a heated scrum at Queen’s Park.
The minister’s comments came after a Star investigation found provincially regulated nursing homes are drugging helpless seniors despite warnings that the powerful antipsychotics can kill elderly patients suffering from dementia.

Ethel Geraldine Anderson (Aunt Gerry) died after being given an antipsychotic drug at a Wellesley St. nursing home. She is the sister of Herb Carnegie, a famous Canadian hockey player.
“What we know is that there are a lot of people being prescribed drugs that raise questions and this work is well underway to make sure that doctors who are prescribing . . . are doing so appropriately,” Matthews told reporters at Queen’s Park. Matthews did not elaborate on what work is being done to ensure appropriate prescribing practices by doctors.
“This is a serious issue, make no mistake about it,” Matthews said. She pointed out that caregivers associated with Behavioural Supports Ontario are doing “fantastic work” controlling the behaviour of people with dementia in nursing homes without drugs. Last year, Ontario invested $43 million in this program.
“It is the way to go and we are going in that direction,” Matthews said.
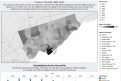
The Star article, published Monday, revealed some long-term care homes, often struggling with staffing shortages, are routinely doling out these risky drugs to calm and “restrain” wandering, agitated and sometimes aggressive patients. At more than 40 homes across the province, roughly half the residents are on the drugs. At close to 300 homes, more than a third of the residents are on the drugs.
NDP Leader Andrea Horwath said Tuesday the Star’s findings were “horrifying.”
At one nursing home east of Ottawa, the Star found, 73 per cent of the residents are on the drugs. A leading drug safety expert on Tuesday called the high rate “madness.”
The head of the long-term care physicians association, Dr. Andrea Moser, did not take issue with the minister’s comments in an interview with the Star.
The use of antipsychotics is “a system issue. You can’t point a finger at one person,” said Moser.
“A lot of good work has been done over the last couple of years. We’re making progress. We still have a long way to go.”
Matthews’ suggestion that the government is not involved in prescribing decisions “outraged” the head of the registered nurses association, Doris Grinspun.
Grinspun said the province can do more to boost training and staffing levels at nursing homes so that caregivers rely less on antipsychotics to control agitation in those with dementia.
“I am, quite frankly, outraged at anyone, let alone the minister, who tries to divert responsibility. It’s all of our responsibility,” Grinspun said.
While doctors ultimately make the decision to prescribe, experts the Star spoke with said it is often done after consulting with long-term care home staff, including nurses and personal support workers, or PSWs.
The medications at issue, including olanzapine, quetiapine and at least 10 others, are not approved by Health Canada for elderly people with dementia. Pharmaceutical companies have issued the strongest possible caution, known as a black-box warning, on their labelling.
“Elderly patients with dementia treated with atypical antipsychotic drugs are at an increased risk of death compared to placebo,” a typical warning says, adding that these patients face a 60 per cent increased risk of death compared with similar patients who are not taking these drugs.
In one of the cases probed by the Star, antipsychotic medication was apparently given to a senior without consent.
Ethel Geraldine Anderson, known as Aunt Gerry to her loved ones, is among such cases reported in the Star investigation. Anderson’s niece said “they tried to quiet her down” with doses of olanzapine in the Wellesley St. nursing home where she was living. Four months later, she was dead.
In a heated scrum with reporters, Matthews said it is clear to her that “doctors cannot prescribe this kind of medication without the consent of the individual or their substitute decision maker.”
Matthews, who cautioned reporters that the information the Star has is “raw data,” added that her government is making investments in care plans that will provide “alternatives to that pharmaceutical solution.”
Nursing homes and the association representing them have also acknowledged the problem and called on the province to act. A fellow member of Matthews’ Liberal government, MPP Donna Cansfield, has said the province must act.
Family members, doctors and, in one case, the provincial coroner believe that prescriptions for these drugs have contributed to the deaths of Ontario seniors with dementia.
France Gelinas, the NDP health critic, said Tuesday the “deadly crisis” must be addressed. “The consequences of excessive prescribing of antipsychotic drugs can and has been deadly.”
The NDP said a 2007 auditor general report warned the government about the overuse of antipsychotic drugs.
“I am shocked that the government has not moved on this issue even though they’ve known about it for some time,” said Horwath.
Several homes with high rates told the Star they are trying to get their prescribing rates down. Where possible, they want to devote resources to “behavioural” therapies, whereby caregivers are trained to identify and neutralize what triggers agitation in residents with dementia. Triggers may include hunger or physical contact in common living areas.
Earlier this year, Health Minister Matthews announced funding to place nurse practitioners in 75 long-term care homes over a three-year period. Grinspun, of the nurses association, said the announcement is a start but more help is needed to address a provincewide problem.
Statistics obtained by the Star show rates of antipsychotic use at 631 nursing homes in the first half of 2013 averaged 33 per cent.
David Bruser can be reached at 416-869-4282 or at dbruser@thestar.ca
Top News
- NEW Murder of Scarborough mother of four tied to 2013 shooting, police say
- Updated Western University student charged over Heartbleed SIN theft
- Power outage caused by Toronto Hydro, HydroOne lines connecting
- Video Family, friends of victims left reeling after Calgary stabbing deaths
- Video Jim Flaherty ‘strode like a giant,’ Stephen Harper says in eulogy
- NEW Criminal Code not the sole boundary for politicians: Hébert
- Witness recalls feeling ‘nailed to the bed’ after drinks, sex assault trial hears
- 3 mandatory vaccines for Ontario children announced












We value respectful and thoughtful discussion. Readers are encouraged to flag comments that fail to meet the standards outlined in our Community Code of Conduct. For further information, including our legal guidelines, please see our full website Terms and Conditions.
If these homes are trying to keep Seniors sedated how do they manage them should an emergency arise requiring the evacuation of the building? I worry that Homes for the Aged are already sedating many of their senior residents at night at their request so they can get a good night sleep but what would happen if a fire broke out and they must get these individuals out of the building quickly? Remember the recent fire in Quebec killing over 30 Seniors who were not able to vacate their building when... » more
Right, blame the third party. Such a common tactic throughout the entire business/political world now. The government creates the rules, pharmaceutical companies are in bed with them, and the doctors are the poor suckers responsible to both. We live in the most gutless of times right now. The people set up for failure are the same ones pieces of crap like Deb Matthews point the finger at when things ultimately hit the fan. Democracy and leadership is under assault in this country
Deb Matthews is one of the most dishonest politicians on the planet. She will say anything not to have to take responsibility for her Ministry. If you were a doctor, on contract to a nursing home, and you had nurses and nursing supervisors coming and telling you that patient X is combative and violent to the staff and other patients, what alternative does the Doctor have? Deb Matthews and her Ministry need to find more funding to open more facilities with more staff, who specialize in the care... » more
The whole system is broken...we can start repairing by ridding ourselves of a minister that is clueless. Note this is discussing psychotic drugs...just imagine what they do for over the counter medications! My family member was being overdosed with 8 extra strength Tylenol per day...every day without authorization. Ensure you look at your loved ones file regularly. Another thing, many facilities charge a dispensing fee for each and every pill...so the abuse may be a tied to, aghast...profite... » more
@wasting away the moments that make up a dull day
clueless Minister is apt. How about Slitherman who helped make this mess. Just look at HIS family. Poor child is going to grow up, well...........then there is our premier and her brother inlaw...........Biggest thing is to promote pride day, right, how about world pride day. That is still 10% of the population.....what about the 90%?
I don't trust anything coming out of the co-chair of the Liberal re-election team's mouth. I think Deb Matthews is in a direct conflict and should resign her position as Minister of Health. Is she saying it is all the doctors fault for prescribing from the position of Minister of Health or from the perspective of re-election?
This is one of the most irresponsible articles ever published by the Star, and if the paper does not retract the story, I will be taking further action. My mother has been in a long term care facility for a very extended period of time with Alzheimers. Without the wonderful care she receives, including the medications prescribed by her doctor, she would not be alive today. These medications are regularly reviewed in meetings with the family, our thoughts are considered, and the medications... » more
Please enlighten us with which facility you are so fortunate to be involved with...as this is the first I have ever heard "without the wonderful care she receives". Wishful indeed.
@WelchB I have personal examples of treatment with Seroquel against the wishes of SDM by law.
Almost impossible to get them off
yes fees for drugs added to bill
It's supposed to be a last resort drug for people who may hurt themselves or others it should not be used for chemical restraint or to keep patients quiet
I have seen what can happen if this drug is used for these purposes and it is brutal
infections and death are side effect
especially in elder patients with dementia
who... » more
With a totally disabled husband being looked after by me in our home (we are both nearly 90 years of age)I can tell you that there is a need for help in cases such as mine.
To this end, I want to suggest that we get rid of half of the high-priced bureaucrats sitting in the hospital administration departments as a start. If efficiency experts (who apparently were hired) could not 'shout' loud enough to bring this fact to the attention of whoever should being making the changes, then our... » more
@changechange
Just look at Mazza and the wall of high heels for his girlfriend......Why is this lunatic not in jail for a long, long time??
At the end of said news conference Deb Matthews pointed out a squirrel running by...
@stanley60007@hotmail.com
was that Guinty in disguise.........
@blueb
lookin for his nuts.
The Star should be commended for exposing this issue. However, they neglected to mention that some seniors are forced against their will and without the consent of their family to take a dangerous anti-psychotic drug as an out-patient, living in their home. It's difficult to fight a false psychiatric diagnosis and hospitals are not legally obligated to inform family about a consent and capacity hearing. After suffering debilitating side-effects, including loss of balance, falls and broken... » more
In my experience with my father's care, the nursing homes are so short staffed that I would guess drugs are used as an alternate (and unacceptable) method of "care-giving". For the government to shirk responsibility is shocking to me. If the homes had a decent budget to work with perhaps the situation could improve. Believe me, there is a very long way to go to make improve Long Term Care facilities in Ontario.